As you know, this term I spent some time researching and writing to you about Dengue Fever, or Bone Break Fever as you call it in Guyana.
This blog is for Carla, Tuwana, and my students who were ill with Dengue Fever as some point during the two years I spent teaching in Port Kaituma:
Why is Dengue such an issue in Guyana? -- What do all of these pictures have in common?
Quick Facts about Dengue Fever:
- 3 billion people in the world are at risk of contracting Dengue Fever
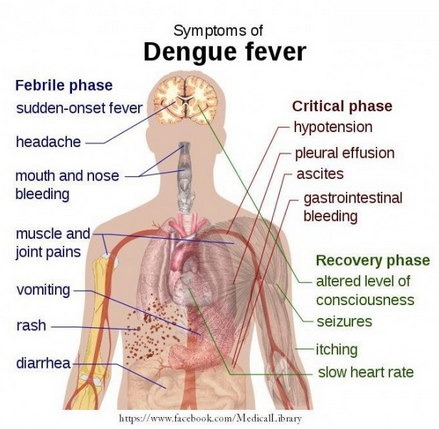
- 1% of the 100 million annual cases of dengue develop into Dengue Hemorrhagic Fever.
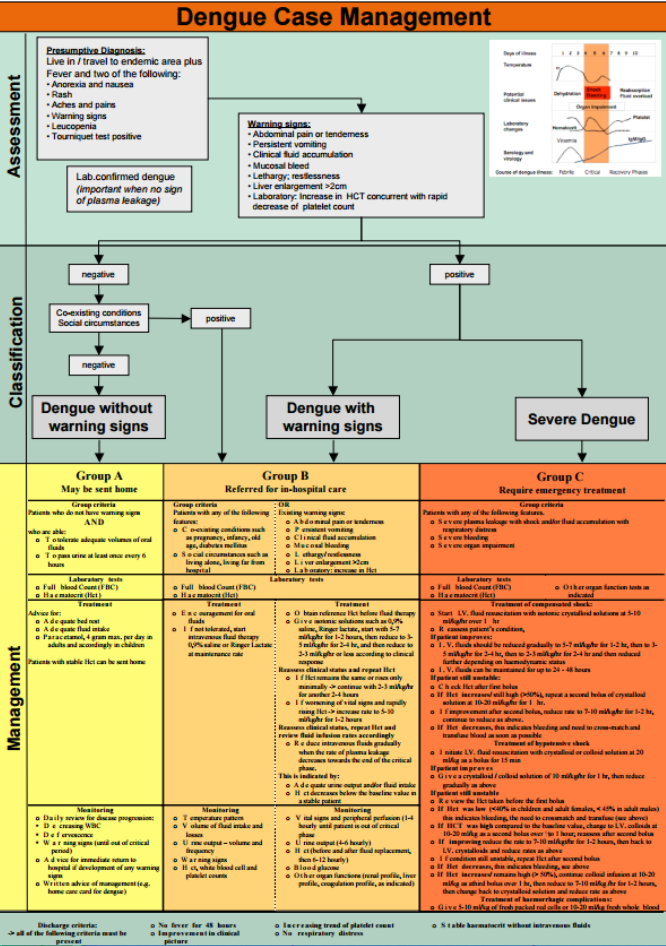
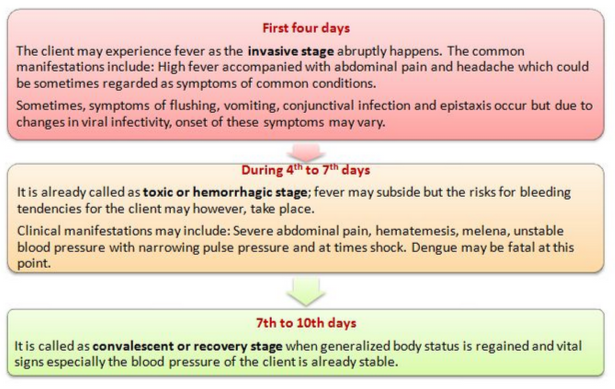
- There is currently no targeted treatment for Dengue Fever -- tylenol and water are the current "standard"
- More research needs to be done to help people who suffer and/or die from this painful condition. Just because it affects people far away doesn't mean the impacts are not real.